From Architecture to AI-Powered Building Diagnostics: Tarek Rakha’s start-up story
10 June 2025
Published online 28 November 2018
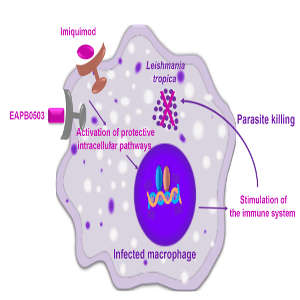
Targeting two of the parasitic species that cause leishmaniasis may soon be possible using an existing drug and a related spin-off.
Hiba El Hajj 2018
A parasitic infection spread by the phlebotomine sandfly, cutaneous leishmaniasis manifests in painful sores, or lesions, on the skin. There are around 20 species of leishmania parasite, and Syria is endemic for both Leishmania major and Leishmania tropica. The recent conflict in the region has led to the rapid spread of the disease to other countries.
“There are various therapeutic interventions that lead to partial or complete cure in L. major lesions but are less effective for L. tropica,” says Hiba El Hajj at the American University of Beirut, who worked on the study with colleagues including Ibrahim Khalifeh, and co-workers at the Université de Montpellier in France. “Furthermore, all existing treatments are associated with high rates of toxicity, high cost, elevated risks of relapse and drug resistance. An effective drug is still out of reach and new strategies must be set.”
The researchers dissected the mechanism of action of a medical cream called Imiquimod, which is currently on the market for treating genital warts. Imiquimod had previously been trialled with some success against L. major, although the molecular mechanisms involved were unclear. Furthermore, they focused their attention on an Imiquimod analog called EAPB0503, which is not yet approved for clinical trial.
The researchers infected cultured macrophages (a type of white blood cell) with both species of leishmania parasite and analysed the effects of the drugs on these cultured cells. They showed that both drugs reduced the replication of both species quickly, within as early as ten hours of treatment. EAPB0503 showed higher efficacy. They then tested Imiquimod and EAPB0503 on freshly collected L. tropica from skin lesions of cutaneous leishmaniasis patients. EAPB0503 showed great promise, proving more potent for L. tropica than previous drug candidates. Both drugs worked quickly to activate a key pathway that triggers host immune responses.
“We plan to collaborate further and formulate a cream with EAPB0503 for topical use,” says El Hajj. “We’re also working on creating in vivo mouse models for cutaneous leishmaniasis; a crucial step ahead of potential clinical trials.”
doi:10.1038/nmiddleeast.2018.146
El Hajj, R. et al. EAPB0503: An Imiquimod analog with potent in vitro activity against cutaneous leishmaniasis caused by Leishmania major and Leishmania tropica. PLOS Negl. Trop. Dis. 12, e0006854 (2018).
Stay connected: