The state of smart cities in MENA
11 December 2025
Published online 11 February 2015
A certain type of T lymphocytes may serve as a reservoir in the body to protect against cancer relapses.
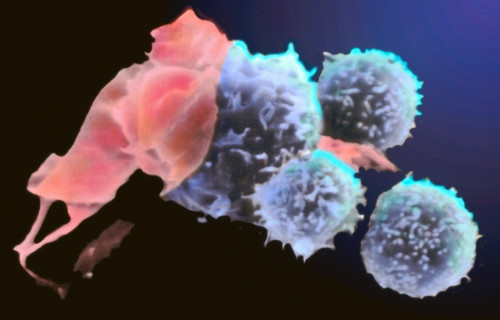
© BSIP SA / Alamy
T lymphocytes are blood cells responsible for attacking cancerous body cells or cells taken over by viruses. In 2011, scientists reported a new subset of T lymphocytes in humans, T memory stem cells (TSCM), which exhibited properties such as self-renewal and differentiation into daughter cells while also sharing the survival capability distinctive of memory cells.
A team of researchers from Italy and Saudi Arabia has now revealed strong evidence that TSCM could be safely and efficiently used for the development of T cell-based therapies.
Until now, T cell properties have mainly been studied through in vitro assays and animal models, so the long-term in vivo fate of T cells in humans is not fully understood.
“TSCM are able to persist in human beings for decades as a reservoir of T cell precursors, maintaining their ability to generate – in vitro and in vivo – memory and effector T cells,” says Luca Biasco, project leader at San Raffaele Telethon Institute for Gene Therapy in Milan, Italy.
The group examined data from two pioneering gene therapy clinical trials that started in the mid-1990s on patients from around the world with a severe congenital immunodeficiency. In the trials, defective T cells were harvested and then corrected with a vector carrying a therapeutic gene. These were then put back into the patients.
“These integration sites act as molecular barcodes that stably mark each engineered T cell and its progeny upon infusion,” explains Biasco. They used these barcodes to trace the fate of different infused T subtypes in vivo, directly, long after infusion.
The team found that gene-corrected TSCM were able to survive in patients up to 12 years after infusion, retaining their potential to differentiate into new blood cells.
“The results of this work are extremely relevant for the design of therapeutic approaches involving T cell engineering,” says Biasco. “This opens the possibility to exploit engineered TSCM as direct targets for T cell-based therapies,” he says, adding that such therapies represent one of the most advanced and promising approaches for the treatment of cancer.
The long-term self-renewal and differentiation properties of TSCM mean they could act as a reservoir of T cells that can activate in case of tumour relapse.
doi:10.1038/nmiddleeast.2015.26
Biasco, L. et al. In vivo tracking of T cells in humans unveils decade-long survival and activity of genetically modified T memory stem cells. Science Translational Medicine. http://dx.doi.org/10.1126/scitranslmed.3010314 (2015)
Stay connected: